2.6 - Documentation of a Serious Illness Conversation / Goals of Care Conversation

Which documentation system do you use?
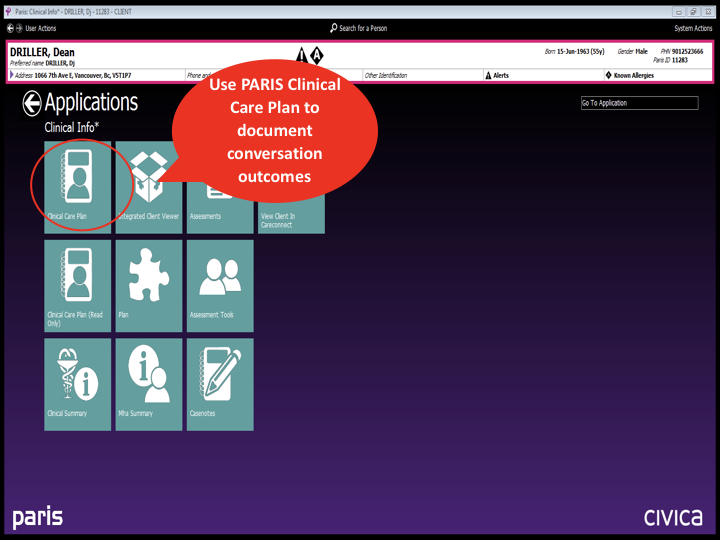
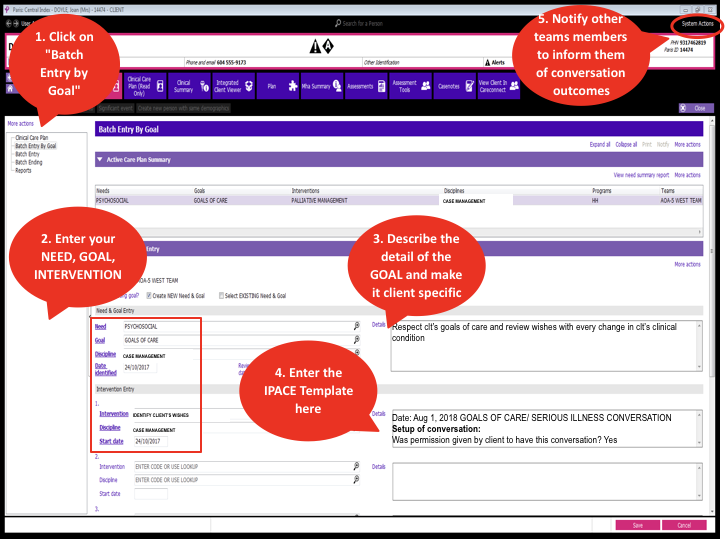
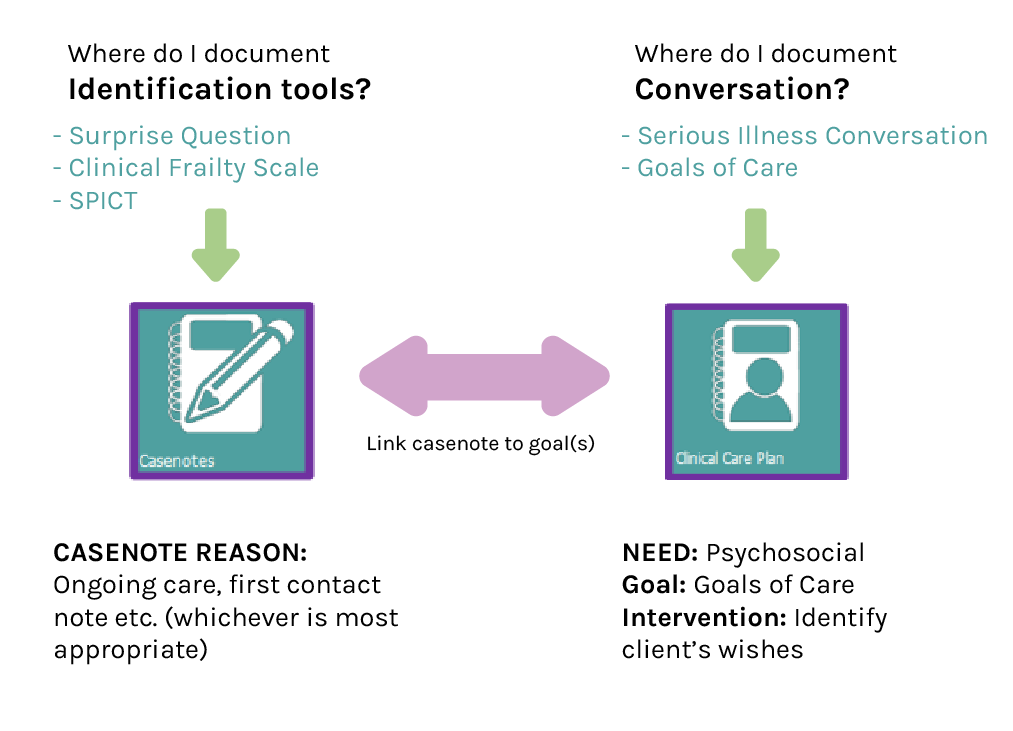
PARIS

If you need a refresher on how to enter clinical care plans, please access the online education Paris 6 VCH Clinical Care Plan (ALL) on the LearningHub.
Download the PARIS Documentation Template from the RPACE Website . All RPACE documentation follows PARIS Guidelines. Please consult your local Clinical Resource Nurse if you have any PARIS related questions.”
Step 1.
Step 2.
Summary
Profile EMR

A. Enter Social History/Risk Problem - SHx 99
*Note that this Problem List including information about ACP gets shared into CareConnect*
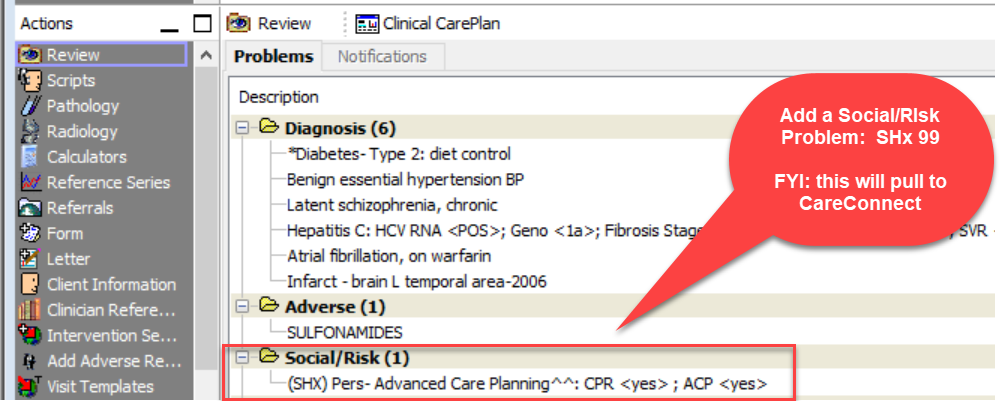
B. Utilize Encounter Note
*No need to use either the Clinical Care Plan or Advance Care Plan Form*

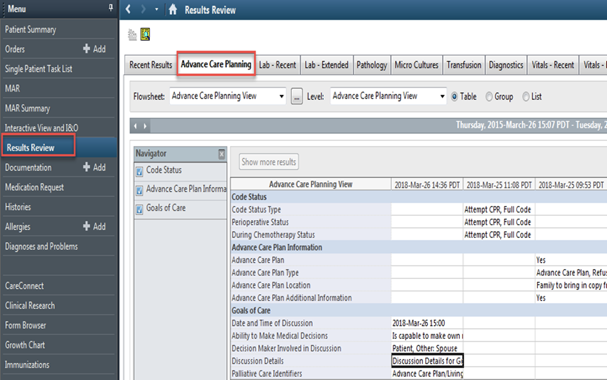
Cerner/CST

You can document GOC conversations in Cerner through several pathways, depending on your user profile:
Results Review — Advance Care Planning
Patient Summary — Handoff Tool
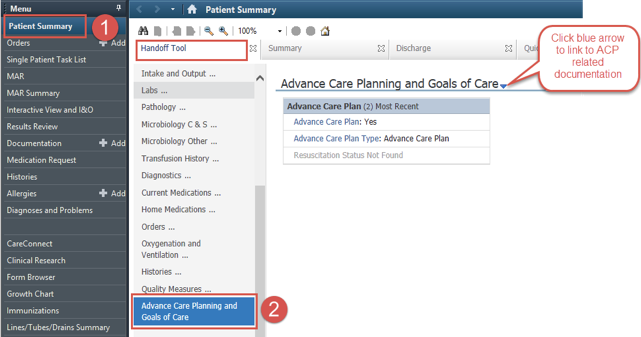
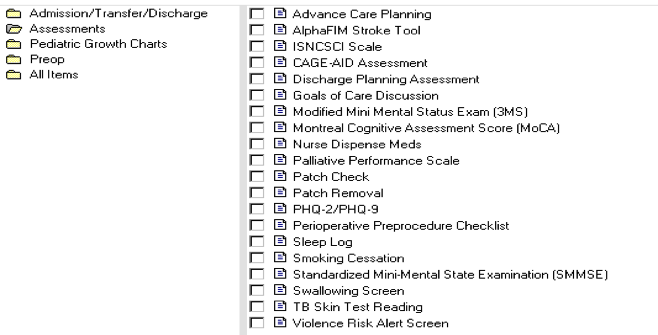
Ad Hoc Forms (Assessment -> Goals of Care Discussion)
Paper Charting

Where paper charting is utilized, all members of the interdisciplinary team are asked to document on the VCH form entitled the Advance Care Planning/Goals of Care Discussion Record (form VCH.0109)
What to document
The clinician should make an entry in the ACP/GOC Discussion Record anytime the patient or Substitute Decision-Maker articulates their wishes, fears, concerns about their prognosis, uncertainty over treatment/decisions, etc… At times this may be a planned conversation that is initiated by the clinician, and in other circumstances, it may be spontaneous conversation that begins with a comment made by the patient or their decision-maker. Any follow-up actions should also be documented.
Ensure that you identify who was involved in the conversation in your entry, and that you sign with your name, discipline, and initials.
Access to the document
This form can be found on the intranet and can be ordered through Printing Services.
Location within the chart
The form is located in the paper chart just before the green sleeve that contains the Medical Orders for Scope of Treatment (MOST) form.
Rationale
The Advance Care Planning/ Goals of Care Discussion Record allows for centralized, multidisciplinary documentation of all information pertaining to a patient’s goals or wishes. The centralization of goals of care documentation allows for rapid access to this vital information, reduces the risk that goals of care charting will be missed within discipline-specific notes, ensures that all members of the team are on the same page, and ensures that the patient’s wishes are respected whenever possible.
In order to avoid double-charting, clinicians can document a brief note in their own discipline’s progress notes directing readers to the documentation: “Please see the ACP/GOC Discussion Record for identification of the need for a goals of care conversation.”
For further information and support on paper documentation of goals of care, there is a short learning module available: "Documentation of Goals of Care in VCH Paper Charts"
Communication
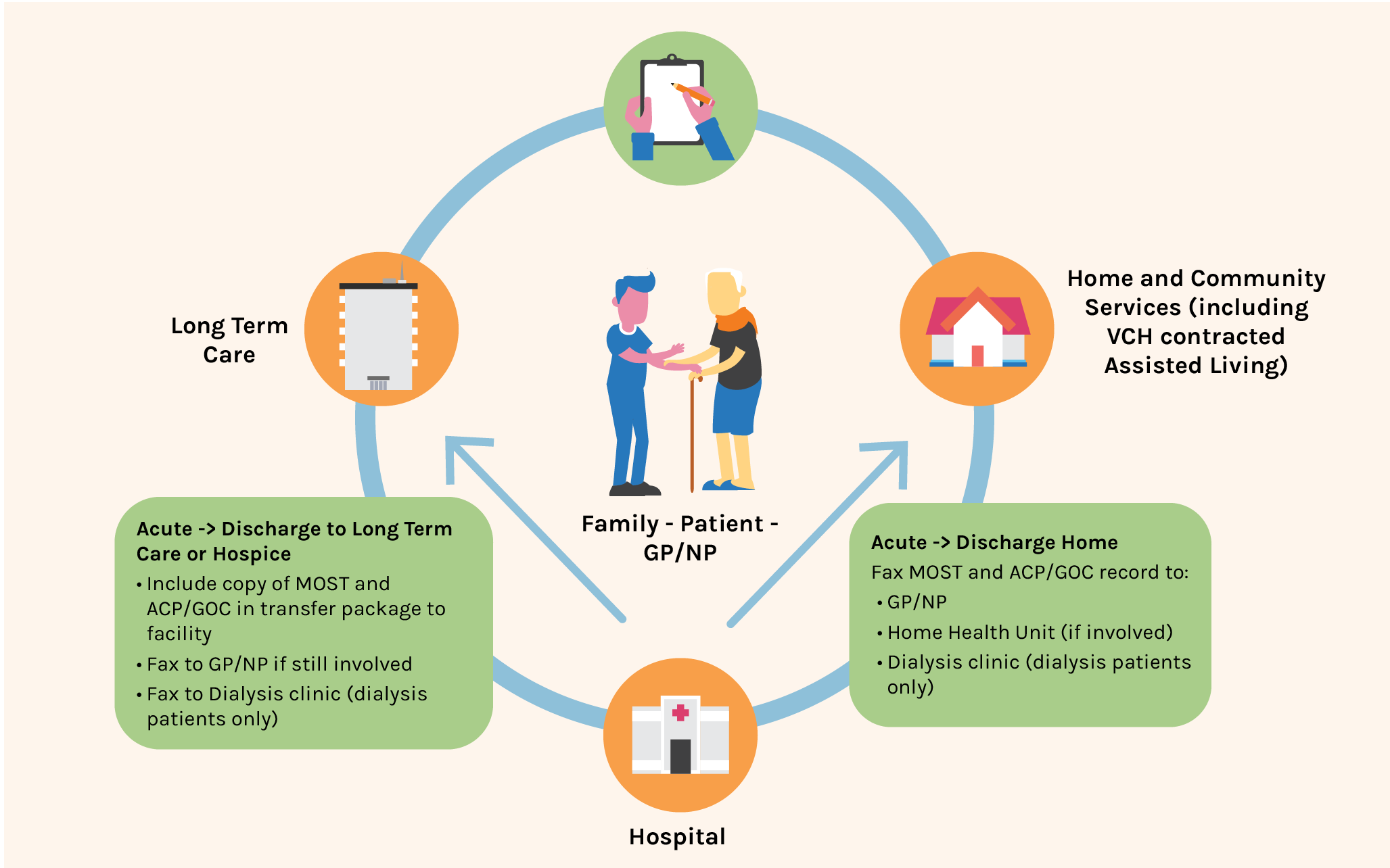
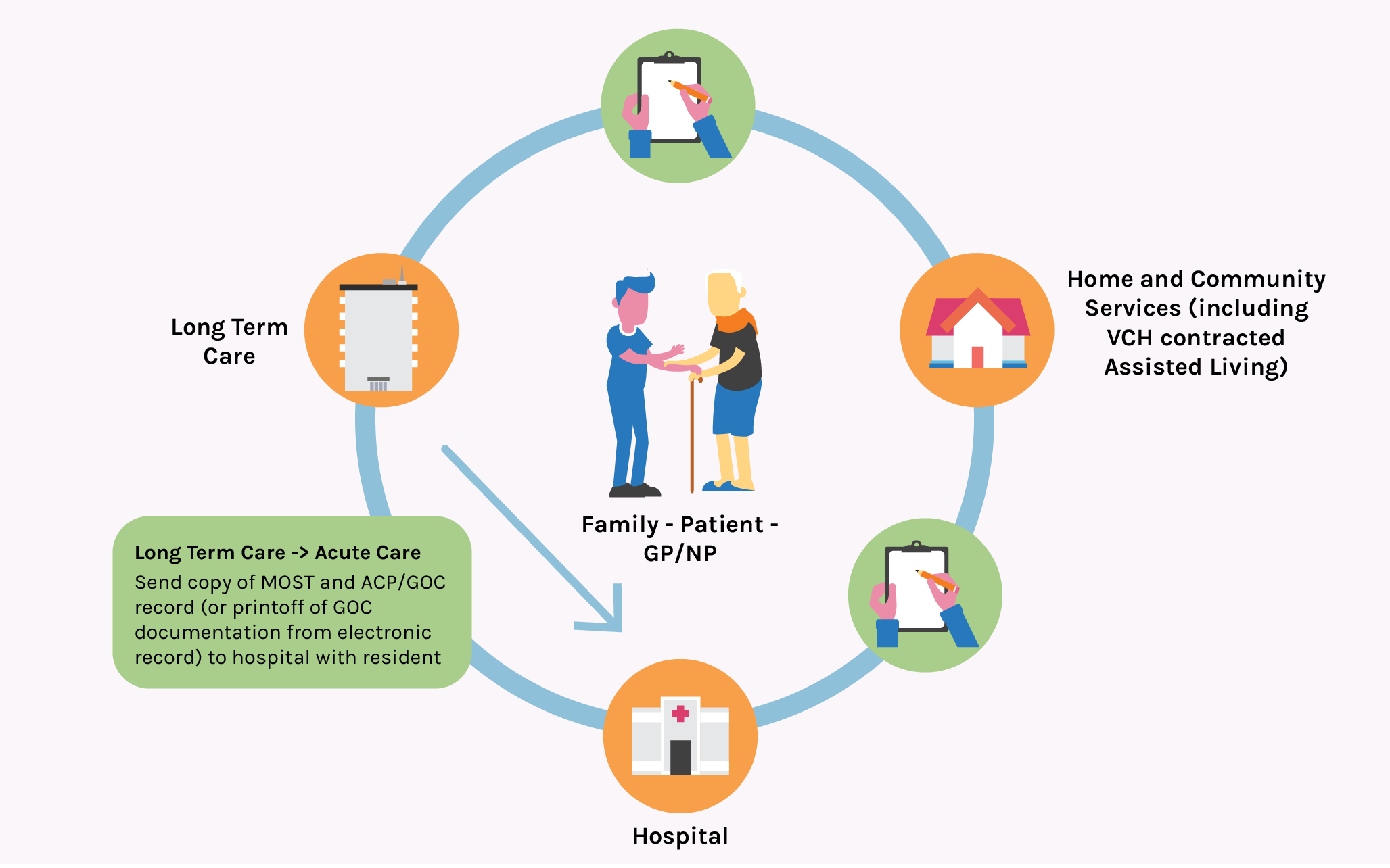
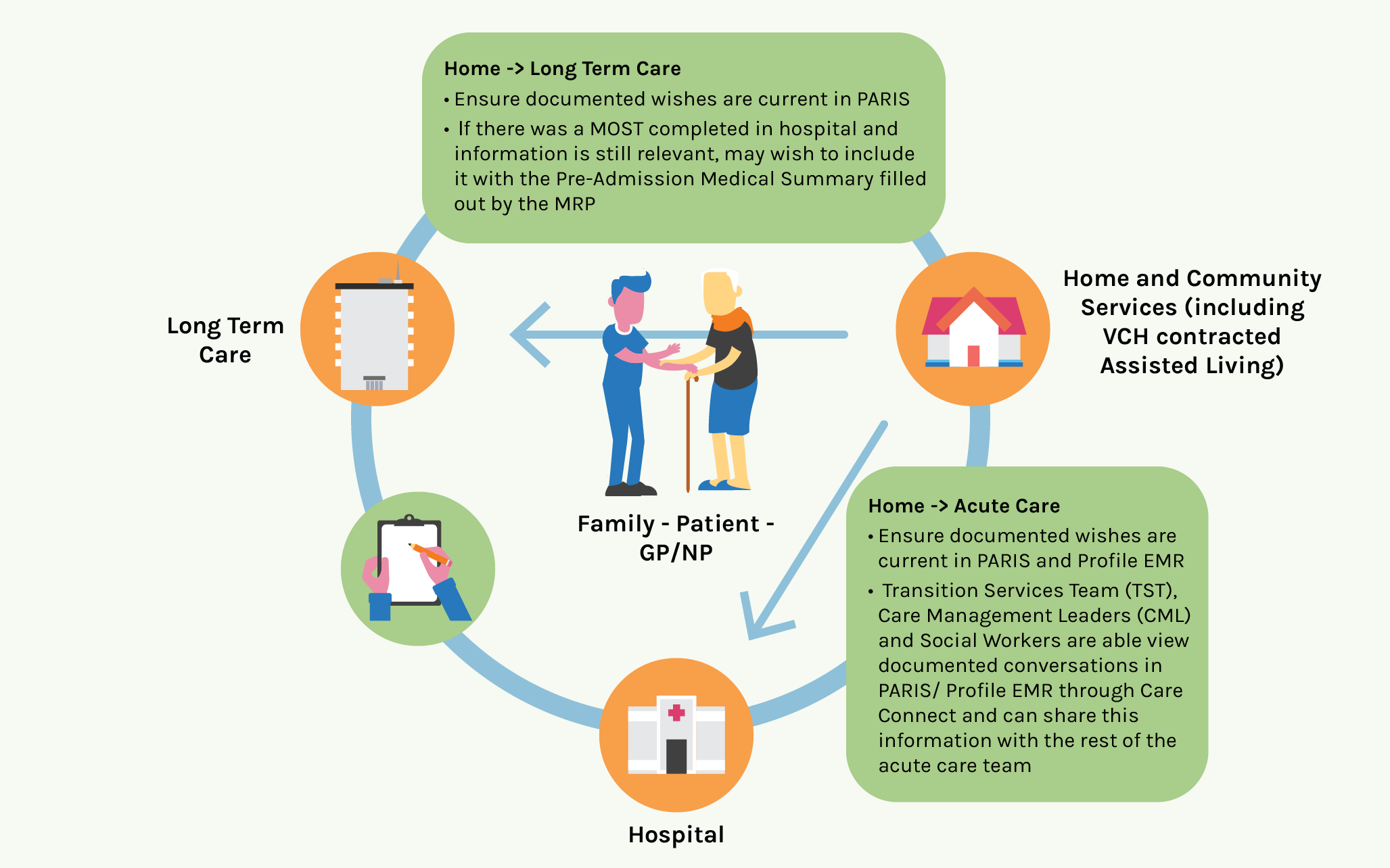
Patients will require a variety of services during the course of their illness. Ensuring a patient's wishes are communicated across the continuum of care allows teams to prioritize care according to people's wishes.
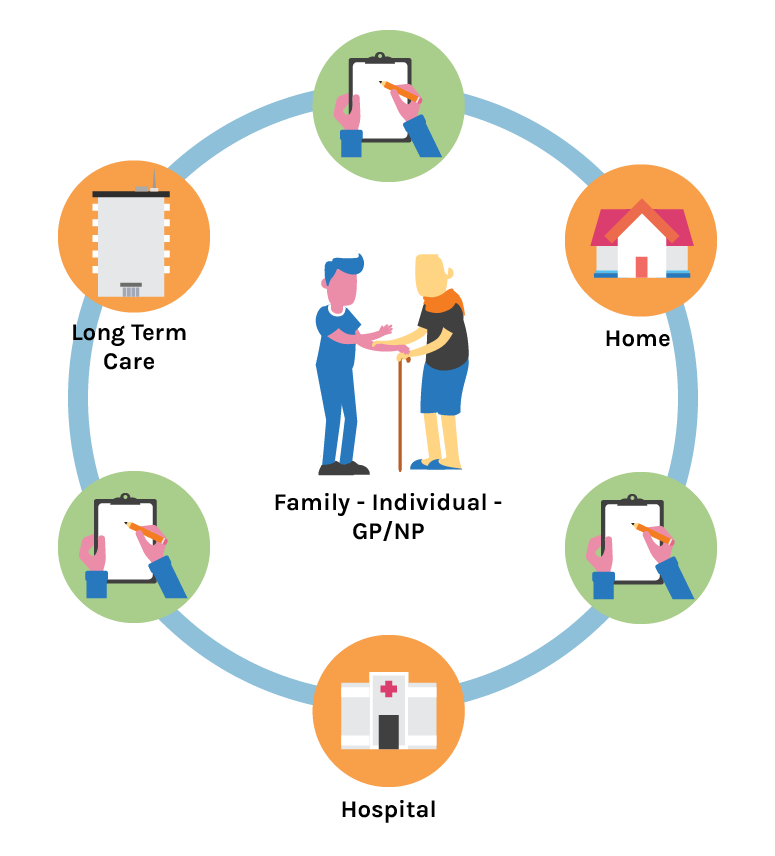

How does information get shared at care transitions?
CareConnect supports continuity of care as patients move across programs and services. This view-only system allows electronic health record users to view a limited amount of patient information documented in another electronic documentation system. This includes documented conversations for certain programs and teams.