1.5 - Identify

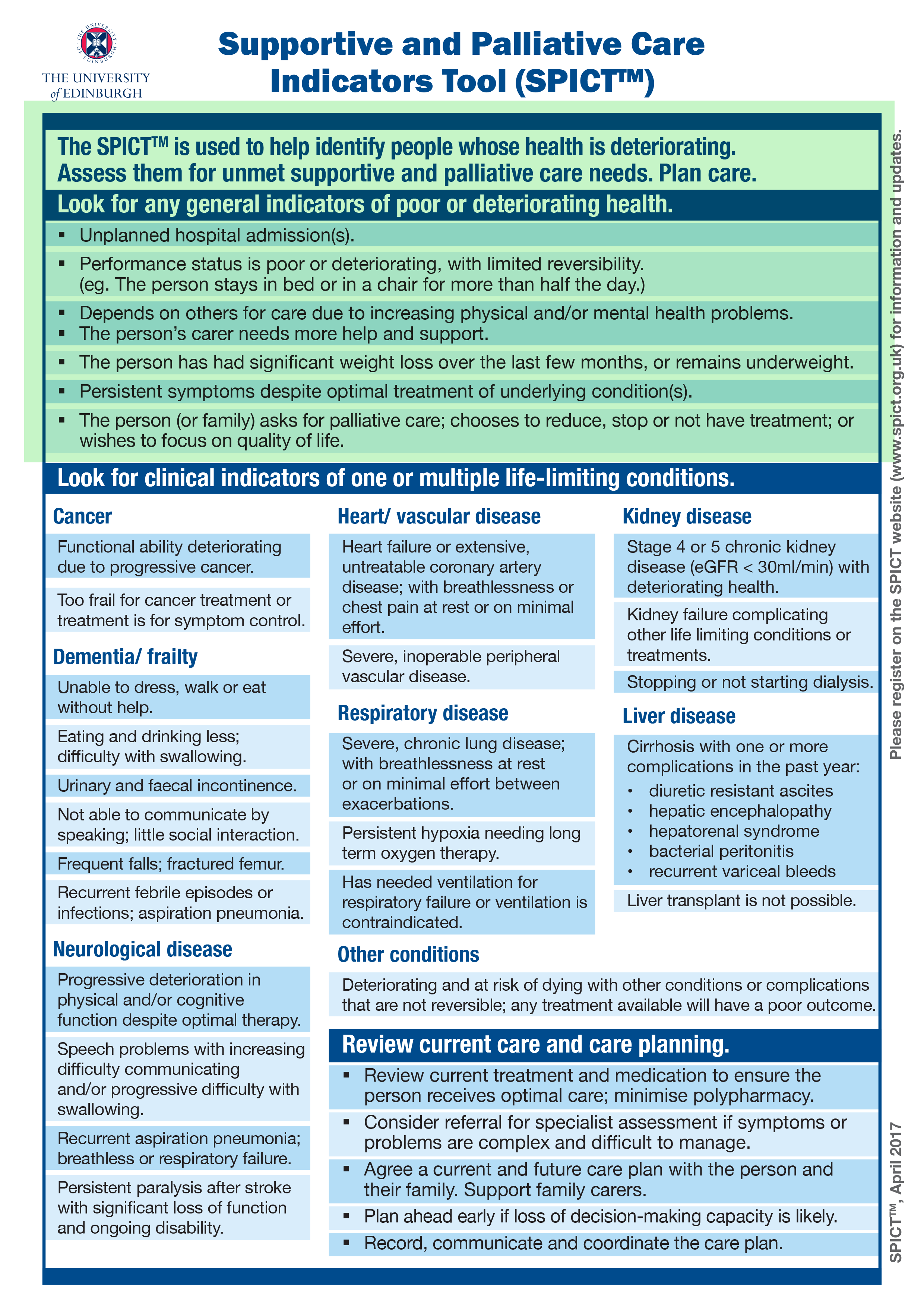
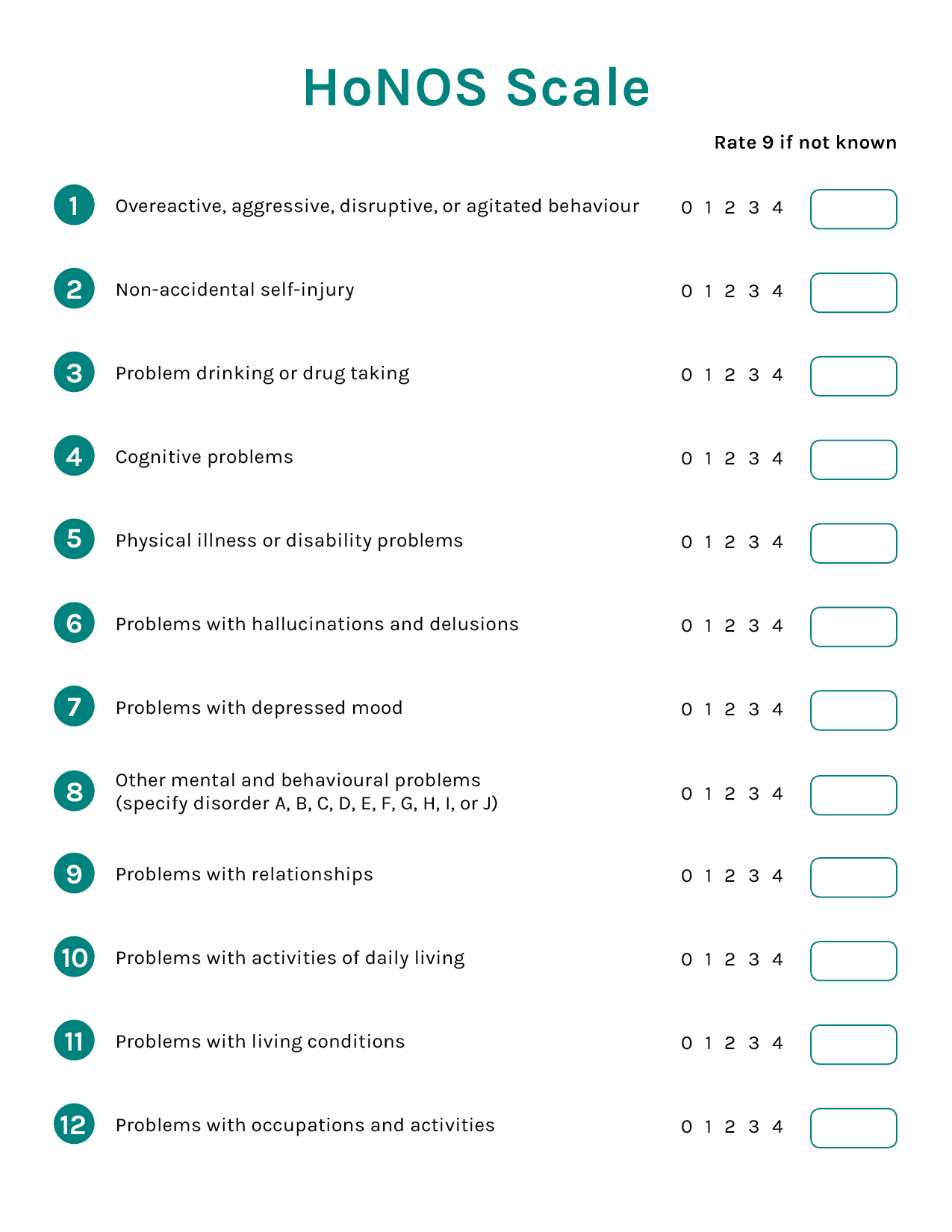
This section will introduce you to several tools that can assist you in identifying which patients would benefit from an early conversation.
1. Surprise Question
Would I be surprised if the patient died in the next 6-12 months?
YES doesn't mean that the patient would not benefit from a palliative approach to care. It is important to go on to other indicators.
NO means that this patient may be at high risk for hospitalization or dying in the next year.
It is important to go on to the other indicators and determine priority.
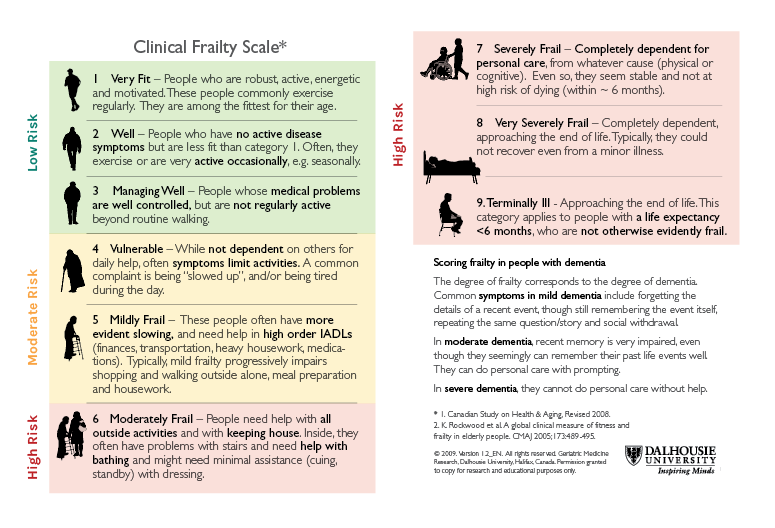
2. Clinical Frailty Scale
The Clinical Frailty Scale is a tool used to assess a patient's instrumental activities of daily living and activities of daily living dependencies, regardless of their diagnosis. Patients who fall into a Moderate Risk or High Risk category should be prioritized for early conversations.
*The Clinical Frailty Scale has not been validated for patients under the age of 65. Please continue to screen patients under 65 using the Surprise Question and the SPICT Tool.
View PDF